Listen to the article
Leading Oncology Organizations Challenge Lung Cancer Screening Misinformation
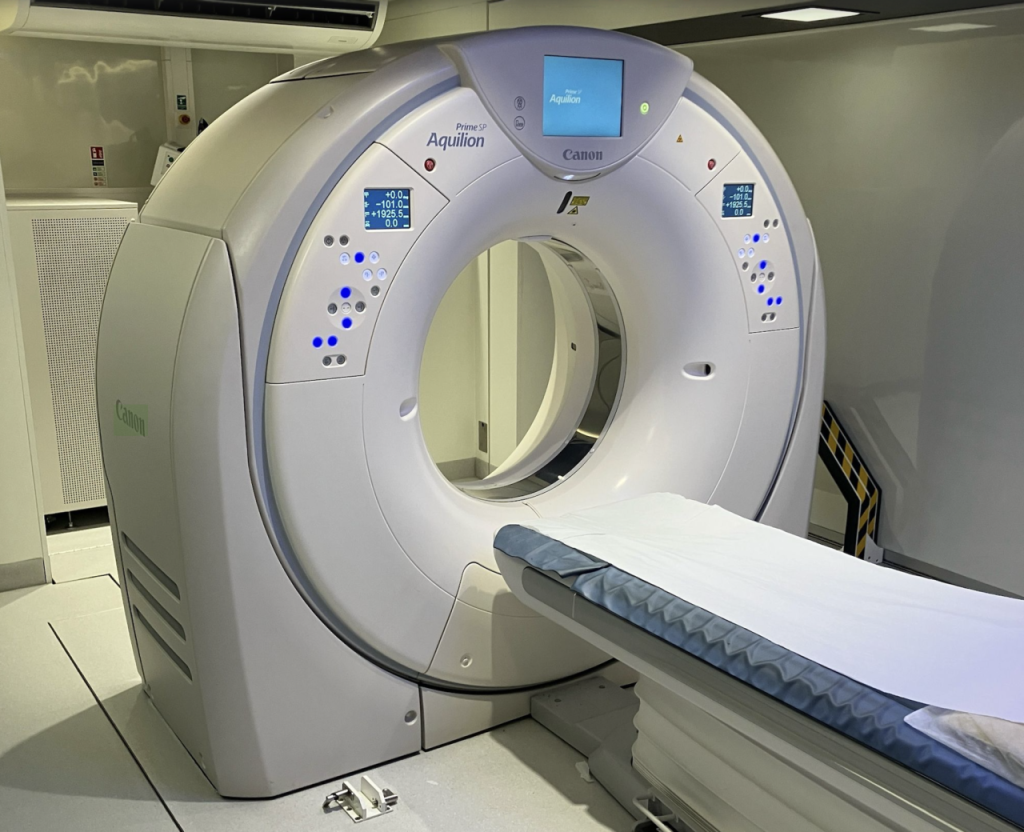
A coalition of prominent American oncology organizations has issued a strong rebuke against what they describe as widespread misinformation about low-dose CT (LDCT) lung cancer screening, warning that inaccurate research is deterring patients from potentially life-saving tests.
The American College of Radiology (ACR), Society of Thoracic Surgeons (STS), and American Society for Radiation Oncology (ASTRO) published a joint letter this month across multiple prestigious medical journals, including the Journal of the American College of Radiology, Annals of Thoracic Surgery, and the International Journal of Radiation Oncology, Biology, Physics.
In their statement, the organizations criticized what they characterized as persistent methodological flaws in recent research that have distorted public and professional understanding about the risks and benefits of lung cancer screening. They argue that certain studies have exaggerated false positive rates and relied on questionable assumptions about radiation risks.
“This overstatement of potential complications is potentially discouraging medical professionals and patients from relying on what they view as a life-saving tool,” the authors wrote. The concern is particularly pressing given that lung cancer remains the leading cause of cancer death in the United States, with early detection strongly correlated with improved survival rates.
The organizations specifically challenged a 2023 study from the University of California, San Francisco, which claimed that CT examinations could account for 5 percent of new cancer cases. That research estimated that the 93 million CT scans performed in 2023 would cause 103,000 new cancer cases.
“An alarming 255 percent increase compared with a prior 2007 modeling despite only a 30 percent increase in CT scans performed and better overall CT scanning technology using lower radiation exposure,” the organizations noted, suggesting that such discrepancies warrant careful scrutiny.
A central criticism targets the methodology behind radiation risk assessments. The letter explains that some researchers inappropriately extrapolate cancer risk data from Japanese atomic bomb survivors to estimate risks from medical imaging procedures. “Associating acute and intense radiation exposure from atomic bombings with cancer risk from CT imaging requires inappropriate extrapolation,” the authors stated.
The letter also highlights confusion in how study results are reported, noting that journalists and advocates have frequently misinterpreted statistical findings. Many have incorrectly cited a 96.4 percent figure from earlier studies in ways that wrongly suggest nearly all positive screening results prove unnecessary, a conclusion the organizations describe as “factually incorrect and misleading.”
The intervention comes at a critical time, as current screening rates remain alarmingly low. Less than one in five eligible individuals undergo recommended annual lung cancer screening, a statistic that has motivated these organizations to address what they view as unfounded fears.
Dr. Drew Moghanaki, a radiation oncologist and vocal advocate for lung cancer screening, commented on social media about the issue, suggesting that misinformation campaigns have historical parallels to tobacco industry tactics that sought to undermine public health initiatives.
The ACR, ASTRO, and STS collectively represent tens of thousands of specialists directly involved in imaging, radiation therapy, and surgical management of lung cancer. Their coordinated effort underscores significant concern about how screening data is being assessed and communicated to both healthcare providers and the public.
While emphasizing that LDCT remains the only screening method proven to reduce lung cancer mortality, the societies acknowledge that the broader screening landscape continues to evolve. Emerging technologies, including breath-based diagnostics platforms, are being developed to complement imaging with additional modalities that may further refine pathways for earlier diagnosis.
This rare consensus statement from leading medical organizations highlights the critical importance of accurate information in healthcare decision-making, particularly for screening programs that have demonstrated mortality benefits for high-risk populations.
Fact Checker
Verify the accuracy of this article using The Disinformation Commission analysis and real-time sources.



10 Comments
I appreciate the medical groups taking a strong stance here. Lung cancer is a serious issue, and patients deserve to have reliable data to guide their healthcare choices.
Agreed. Misinformation can be very harmful, especially when it comes to critical health decisions.
I’m curious to learn more about the specific issues the organizations have identified with the recent research on lung cancer screening. What methodological flaws did they find?
That’s a good question. The article mentions concerns about exaggerated false positive rates and questionable assumptions about radiation risks. It would be helpful to see the details of their critique.
Glad to see these leading medical groups taking action to counter misinformation. Accurate information is so important, especially for potentially life-saving procedures like cancer screening.
This is an important reminder that we need to be vigilant about medical research and reporting. It’s easy for flawed studies to spread and mislead the public.
This highlights the ongoing challenge of combating misinformation in the digital age. It’s critical that authoritative sources provide clear, evidence-based guidance to the public.
Absolutely. Misinformation can have real and serious consequences, so it’s crucial that trusted medical organizations take a strong stand against it.
Interesting to see leading oncology groups push back against misinformation on lung cancer screening. Seems like they are concerned that exaggerated risks could deter patients from potentially life-saving tests.
Yes, it’s important to have accurate information about the benefits and risks of screening to ensure patients make informed decisions.