Listen to the article
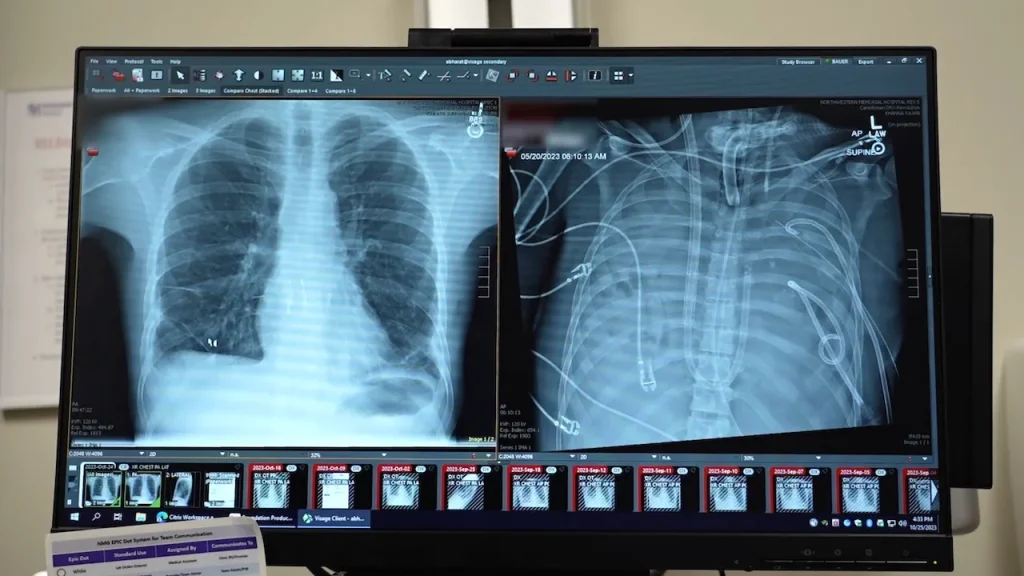
In a groundbreaking medical achievement, surgeons at Northwestern Medicine in Chicago successfully kept a 33-year-old patient alive for 48 hours after removing both of his lungs. The Missouri resident, whose name has not been disclosed, was initially transported to Northwestern Memorial Hospital in spring 2023 with severe lung failure resulting from a flu infection.
The patient’s condition rapidly deteriorated into severe pneumonia and sepsis, causing his heart to stop and requiring CPR, according to the hospital’s press release. Dr. Ankit Bharat, chief of thoracic surgery and executive director of the Northwestern Medicine Canning Thoracic Institute, explained the severity of the situation.
“He had developed an infection of his lungs that just could not be treated with any antibiotics because it was resistant to everything,” Dr. Bharat said. “That infection caused his lungs to liquify and then continued to progress to the rest of his body.”
The medical team faced a critical dilemma: the infected lungs needed to be removed immediately to prevent the spread of the life-threatening infection, but doing so posed an extreme risk of immediate heart failure.
“The lungs act as a ‘shock absorber’ for the right side of the heart; when you remove them, the heart pumps against high resistance and can fail instantly,” Dr. Bharat explained. “Another critical danger is that without blood flowing from the lungs to the left heart, the left heart chambers can collapse or form deadly clots.”
To overcome these challenges, the surgical team designed an innovative “total artificial lung system” (TAL) that could temporarily take over the vital functions of the lungs while the patient awaited a transplant. This system maintained blood oxygenation, removed carbon dioxide, and preserved critical blood flow to the heart.
What made this approach particularly revolutionary was its design philosophy. “A key innovation here is that we maintained the heart’s natural physiology. By using a ‘flow-adaptive’ design, we allowed the patient’s own heart to regulate blood flow, rather than forcing it with a machine,” Dr. Bharat noted.
The strategy proved immediately effective. “Just one day after we took out the lungs, his body started to get better because the infection was gone,” Dr. Bharat said. After the 48-hour period without lungs, the patient was stable enough to undergo a double-lung transplant.
This case represents the first successful application of this specific type of artificial lung system. While similar concepts have been attempted in rare cases historically, previous efforts faced significant limitations in managing blood flow and preventing dangerous clots.
“Our system is novel because it includes a self-regulating ‘shunt’ that mimics the natural physics of the lung to protect the heart, and it uses dual return tubes to maintain normal blood flow through the left heart chambers,” Dr. Bharat explained.
The details of this remarkable case were published last week in the Cell Press journal Med. The study included a molecular analysis of the removed lungs, revealing extensive scarring and tissue damage. This finding supports the notion that in some severe cases of acute respiratory distress syndrome, transplantation may be the only viable treatment option.
Two years after the procedure, the patient has made a remarkable recovery. “The patient is doing remarkably well,” Dr. Bharat reported. “He has excellent lung function, his heart function is preserved and he is completely functionally independent.”
The medical team hopes that this innovative TAL system could eventually provide a lifeline for patients awaiting donor lungs, particularly those suffering from severe acute respiratory distress syndrome (ARDS) with complications like necrotizing pneumonia or septic shock.
“These patients have a mortality rate exceeding 80% and are often turned down for transplant because they are too infected,” Dr. Bharat said. “This technology allows us to ‘clean the slate’ by removing the infection, stabilizing the patient and bridging them to a successful transplant.”
Looking ahead, Dr. Bharat and his team envision developing durable, implantable artificial lungs that patients could live with long-term, not just as a temporary bridge to transplantation. This could potentially transform treatment options for those with end-stage lung disease and expand the possibilities for patients who might otherwise have no viable treatment options.
Fact Checker
Verify the accuracy of this article using The Disinformation Commission analysis and real-time sources.



16 Comments
Incredible medical achievement! Pioneering a new lung transplant approach to save a critically ill patient’s life is remarkable progress. I’m curious to learn more about the technology and techniques used to sustain the patient without lungs for 48 hours.
Agreed, this is a significant breakthrough that could have major implications for lung transplants and patient care. The medical team’s ability to innovate and adapt to save this patient’s life is truly impressive.
While this is an incredible medical feat, I wonder about the long-term viability and risks of this approach. Keeping a patient alive without lungs for 48 hours is remarkable, but could this be a sustainable solution for lung transplants going forward?
That’s a good point. The long-term sustainability and safety of this technique will be crucial as it is further developed and potentially applied more broadly. Careful monitoring and follow-up will be essential.
This is an impressive medical achievement, but I have some concerns about the long-term viability and potential risks of this approach. While keeping a patient alive for 48 hours without lungs is remarkable, is this truly a sustainable solution? Careful evaluation and further research will be crucial to understand the full implications.
Those are valid points. The long-term safety and feasibility of this technique will need to be thoroughly assessed before it can be widely adopted. Ongoing monitoring and continued development of the technology will be essential to understand the true potential and limitations of this approach to lung transplants.
This is a remarkable breakthrough in medical technology and patient care. The ability to sustain life without functioning lungs, even temporarily, opens up new possibilities for treating end-stage lung disease. I’m curious to see how this approach evolves and is applied in the future.
Absolutely, this is a game-changer for lung transplants and patient outcomes. The medical team’s innovation and problem-solving skills are truly inspiring. I look forward to seeing how this technology progresses and benefits more patients in need.
This is an incredible medical achievement, but I have some concerns about the broader implications. While keeping a patient alive for 48 hours without lungs is remarkable, is this truly a sustainable long-term solution? What are the potential risks and complications that could arise?
Those are valid concerns. The long-term viability and safety of this approach will need to be thoroughly evaluated before it can be widely adopted. Careful monitoring and further research will be crucial to understand the full implications and limitations of this technology.
This is a remarkable medical achievement, but I have some concerns about the broader implications and long-term sustainability of this approach. While keeping a patient alive for 48 hours without lungs is impressive, what are the potential risks and complications that could arise? Careful evaluation and further research will be crucial.
Those are valid points. The long-term viability and safety of this technique will need to be thoroughly assessed before it can be widely adopted. Ongoing monitoring and further development will be essential to understand the full potential and limitations of this approach to lung transplants.
Wow, this is a remarkable medical breakthrough! Keeping a patient alive for 48 hours without functional lungs is an incredible feat of innovation and problem-solving. I’m curious to learn more about the specific techniques and technologies used to sustain the patient in this case.
Agreed, this is a groundbreaking development in the field of lung transplants and critical care. The ability to sustain life without lungs, even temporarily, opens up new possibilities for treating end-stage lung disease. I look forward to seeing how this technology evolves and is applied in the future.
Incredible medical breakthrough! Sustaining a patient’s life for 48 hours without functional lungs is an astonishing feat of innovation and problem-solving. I’m eager to learn more about the specific techniques and technologies used to achieve this remarkable outcome.
Agreed, this is a groundbreaking development that could have significant implications for the future of lung transplants and critical care. The medical team’s ability to think creatively and adapt to save this patient’s life is truly inspiring. I look forward to seeing how this technology evolves and is applied more broadly.