Listen to the article
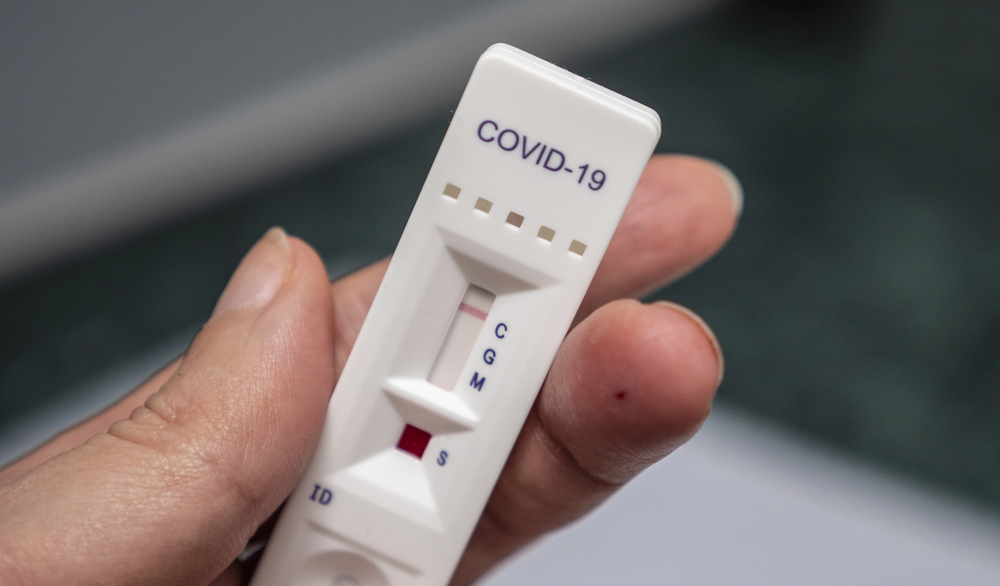
Oklahoma authorities have reached a settlement agreement with nine pharmacies accused of improperly billing the state’s Medicaid program for COVID-19 testing. Attorney General Gentner Drummond announced Tuesday that the pharmacies will pay a combined $157,000 to resolve allegations they submitted unauthorized claims to SoonerCare for over-the-counter COVID-19 tests.
The pharmacies named in the settlement include Apothecary Pharmacy, Cornwell Pharmacy, Cushing Family Pharmacy, R.T.’s Family Discount Pharmacy, Foster Corner Drug, Tiger Drug, Yale Drug, Jones Drug Store, and Swipht Pharmacy. All nine establishments came under scrutiny following an investigation conducted by the state’s Medicaid Fraud Control Unit.
“I appreciate the careful and extensive work by my investigative team to recover these funds,” Drummond said in a statement. “I take seriously all allegations of false claims and am committed to holding anyone who abuses the system accountable to the law.”
The case marks a significant development in Oklahoma’s ongoing efforts to combat healthcare fraud and protect taxpayer dollars, particularly those allocated for public health programs like SoonerCare, Oklahoma’s Medicaid program that provides healthcare coverage for low-income residents.
The settlement comes amid heightened scrutiny of COVID-19 related healthcare billing across the country. During the pandemic, federal and state governments expanded coverage for COVID-19 testing to ensure widespread accessibility, but this also created opportunities for improper billing practices.
Healthcare fraud has remained a persistent issue throughout the pandemic, with the Department of Health and Human Services Office of Inspector General reporting billions in questionable billing nationwide related to COVID-19 testing, treatment, and prevention measures.
For Oklahoma’s SoonerCare program, which serves approximately 1.2 million residents, including children, pregnant women, and adults with limited financial resources, maintaining fiscal integrity is crucial. The program operates with strict guidelines about which services can be billed and by whom.
The specific allegations against the nine pharmacies centered on hundreds of unauthorized claims for over-the-counter COVID-19 tests. While many tests were eligible for reimbursement through Medicaid programs during the public health emergency, strict protocols governed how these tests should be administered and billed.
Assistant Attorney General Jamie Bloyd led the investigation alongside agents Justin Brown and Daniel Shcolnik from the Attorney General’s Medicaid Fraud Control Unit. The unit is responsible for investigating and prosecuting Medicaid provider fraud, as well as abuse or neglect of Medicaid beneficiaries in Oklahoma.
The settlement demonstrates the state’s commitment to protecting public health resources during a time when healthcare systems face unprecedented challenges. It also serves as a reminder to healthcare providers about the importance of adhering to proper billing practices, even during public health emergencies.
Industry analysts note that independent pharmacies have faced significant financial pressures throughout the pandemic, balancing increased demand for services with complex reimbursement systems. However, regulatory compliance remains essential regardless of market conditions.
This case also highlights the broader tensions within healthcare billing systems, where complex regulations and rapidly changing guidelines during the pandemic created potential confusion about proper billing procedures.
The recovered funds will be returned to Oklahoma’s Medicaid program, helping ensure that resources remain available for legitimate healthcare needs among the state’s vulnerable populations. The settlement contains no admission of liability by the pharmacies involved.
State officials have not indicated whether additional investigations into COVID-19 related billing practices are ongoing, but the case demonstrates Oklahoma’s commitment to maintaining oversight of healthcare providers receiving public funds.
Fact Checker
Verify the accuracy of this article using The Disinformation Commission analysis and real-time sources.



12 Comments
It’s disheartening to see pharmacies engaging in improper billing practices. But I’m glad the authorities were able to uncover the fraud and take action to recover the misused funds.
This settlement sends a clear message that healthcare fraud will not be tolerated. It’s important for the public to have confidence that Medicaid funds are being used responsibly and for their intended purpose.
It’s disappointing to see pharmacies taking advantage of public health programs. But I’m glad the state is taking swift action to recoup the funds and hold the offenders accountable.
Pharmacies must be held accountable for any improper billing practices. It’s good to see the state taking action to recover misused Medicaid funds and deter future fraud. Protecting public healthcare programs is crucial.
Improper billing practices undermine the public’s trust in the healthcare system. This settlement is a positive step, but ongoing monitoring and enforcement will be crucial to deter future abuses.
While the details are concerning, I’m encouraged to see the Oklahoma Attorney General’s office taking such a proactive stance against Medicaid fraud. Vigilance is key to protecting limited healthcare resources.
Kudos to the investigators for their diligent work uncovering these allegations. Rooting out healthcare fraud is important to ensure taxpayer dollars are used responsibly and patients receive proper care.
Absolutely. Maintaining the integrity of Medicaid is vital, and settlements like this help send a strong message that abuse will not be tolerated.
Pharmacies that abuse the public trust by misusing Medicaid funds should face serious consequences. Kudos to the investigators for their diligence in uncovering this fraud and recovering the stolen funds.
Kudos to the investigators for their diligent work in uncovering this alleged fraud. Holding pharmacies accountable for improper billing practices is essential for protecting the integrity of Medicaid and other public healthcare programs.
Protecting taxpayer-funded healthcare programs like Medicaid is essential. This settlement demonstrates that the state takes these allegations seriously and will not tolerate fraudulent activity.
While the details are concerning, I’m glad to see the state taking swift action to address the alleged fraud. Maintaining the integrity of public healthcare programs is crucial for ensuring patients receive proper care.